Understanding Brain Tumours
Understanding Brain Tumor Resection: A Simplified Guide to Brain Surgery

A diagnosis of a brain tumor can be overwhelming, but understanding the surgical procedure to remove it can help demystify the process. Brain tumor resection, also known as craniotomy, is a highly advanced surgical procedure aimed at removing as much of the tumor as possible while protecting the patient’s brain function. This guide provides a simplified, scientific overview of the procedure, its goals, and what to expect.
The Surgical Goal: Why is Brain Surgery Performed?
The primary objective of brain tumor surgery is to achieve the best possible outcome for the patient. Surgeons have several goals:
- Complete Resection: To remove the entire tumor if it is located in a non-critical area. This is often the ideal outcome.
- Partial Resection: If the tumor is near sensitive areas controlling functions like speech or movement, the surgeon will remove as much of it as safely possible. This relieves symptoms and makes subsequent treatments like chemotherapy or radiation therapy more effective.
- Biopsy: When a complete or partial resection isn’t feasible, a small tissue sample is taken. This biopsy helps pathologists determine the tumor type and grade, which is crucial for developing the correct cancer treatment plan.
- Symptom Relief: Removing a tumor can alleviate pressure inside the skull, reducing symptoms such as headaches, seizures, and nausea.
Step-by-Step: The Brain Tumor Removal Procedure

The surgery is a meticulously planned and executed process involving a team of highly skilled professionals.
1. Preoperative Planning Before the surgery, the patient undergoes advanced imaging scans, typically Magnetic Resonance Imaging (MRI) and Computed Tomography (CT). These scans create a detailed 3D map of the brain, allowing the surgical team to precisely pinpoint the tumor’s location. This information is loaded into a neuronavigation system, acting like a GPS for the brain to help the surgeon navigate during the procedure.
2. Anesthesia and Preparation The patient is given general anesthesia to ensure they are unconscious and pain-free throughout the surgery. The surgical team carefully monitors all vital signs. A small portion of the patient’s hair is shaved at the incision site, and the scalp is disinfected.
3. The Craniotomy: Accessing the Brain This is the core of the procedure:
- An incision is made in the scalp.
- A special surgical drill is used to make a small hole in the skull.
- Using a specialized saw, the surgeon carefully cuts and lifts a “window” of bone, known as a bone flap. This piece is safely stored.
- The dura mater, the tough membrane protecting the brain, is opened to expose the brain’s surface.
4. The Tumor Resection: Precision and Technology This is the most delicate phase. Surgeons use cutting-edge technology to ensure maximum safety and precision:
- Surgical Microscope: Magnifies the surgical field, allowing the surgeon to see fine details and differentiate between the tumor and healthy tissue.
- Intraoperative Neuronavigation: The surgeon’s instruments are tracked in real-time on a screen, showing their exact position relative to the tumor and critical brain structures.
- Functional Brain Mapping: In some cases, the patient may be briefly awakened during the surgery (awake brain surgery) to test functions like speech or movement. This helps the surgeon avoid damaging these critical areas.
- Intraoperative Imaging: An MRI or ultrasound may be performed during the surgery to confirm that as much of the tumor as possible has been removed.
5. Closure Once the tumor is removed, the surgeon meticulously closes the surgical site. The dura mater is sutured, the bone flap is put back in place and secured with small titanium plates and screws, and the scalp is closed with sutures or staples.
Advanced and Alternative Techniques

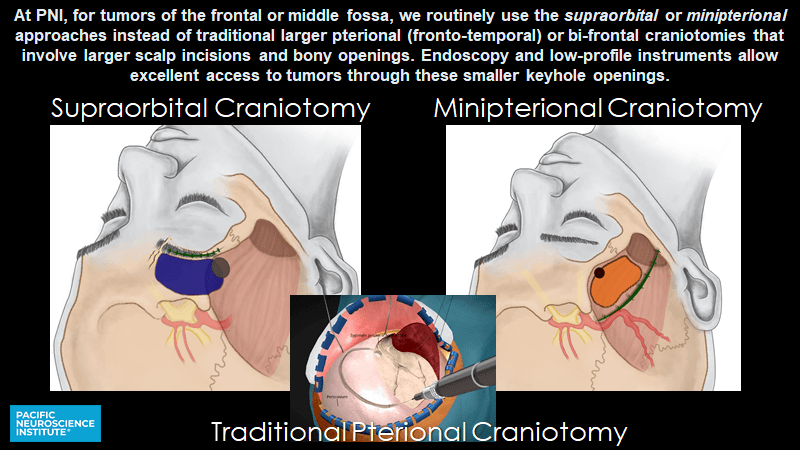
In some cases, less invasive techniques are used, such as:
- Endoscopic Brain Surgery: A thin, flexible endoscope is inserted through a small incision or even the nose to reach the tumor.
- Gamma Knife Radiosurgery: This is not traditional surgery. It uses highly focused radiation beams to destroy a small tumor without any incisions.
- Laser Interstitial Thermal Therapy (LITT): A laser probe is inserted into the tumor to heat and destroy it, with the process monitored in real-time by MRI.
Risks and Recovery
Like any major surgery, brain tumor resection carries risks, including infection, bleeding, or potential damage to healthy brain tissue, which can lead to problems with speech, vision, or movement.
Recovery is a gradual process. Patients typically spend a few days in the hospital, often with time in the Intensive Care Unit for close monitoring. Rehabilitation with physical, occupational, and speech therapy is often a crucial part of the recovery process. Regular follow-up MRIs are essential to monitor for any signs of tumor recurrence.
Brain tumor surgery is a testament to the advancements in modern medicine, offering patients a path to improved health and quality of life.