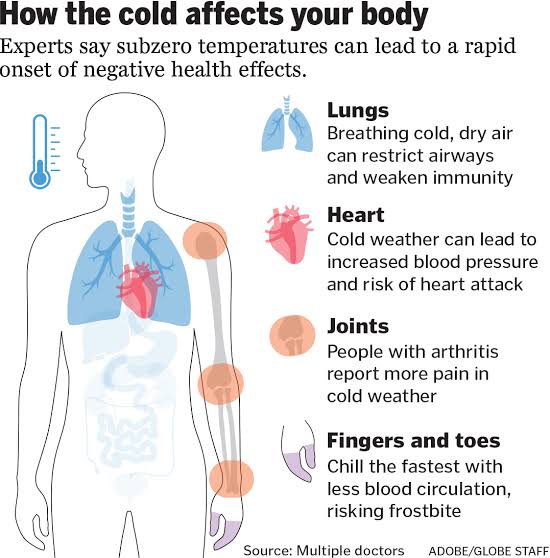
Back pain is considered chronic if it lasts for three months or more. It can come and go, often bringing temporary relief followed by frustration. Dealing with chronic back pain can be especially difficult if you don’t know the cause.
According to hopkinsmedicine, chronic back pain is usually age-related, but it can also result from a previous injury. The most common causes include:
Spinal osteoarthritis – gradual thinning of the cartilage within the spine
Spinal stenosis – narrowing of the spinal canal that can lead to nerve pain
Disc problems, such as a herniated disc or a bulging disc
Myofascial pain syndrome – unexplained muscle pain and tenderness
In some cases, it is difficult to determine the cause of chronic back pain. “If your doctor has exhausted all diagnostic options, it may be time to get a second opinion from a back pain specialist.”
It is important not to make hasty decisions or undergo extensive medical procedures until the source of the pain is discovered. If the source of the pain is unknown or cannot be treated, your best option may be to work with your doctor to reduce your pain episodes and make the pain manageable with nonsurgical treatments.
What non-surgical treatments for chronic back pain?
– Physical therapy
Exercise is the foundation of chronic back pain treatment, and it’s one of the first treatments you should try under the supervision of your doctor and spine physiotherapist. However, the same set of exercises doesn’t work for everyone. Exercise should be tailored to your specific symptoms and condition. An at-home workout routine is also a big part of being successful.
Physical therapy for chronic back pain may include:
Retrain your posture
Pain tolerance test
Stretching and flexibility exercises
Aerobic exercises
Basic reinforcement
Mindfulness and meditation
Chronic back pain results in physical and emotional stress. To manage frustration, irritability, depression, and other psychological aspects of dealing with chronic pain, you may be referred to a rehabilitation psychiatrist. This specialist may recommend meditation, yoga, tai chi, and other cognitive and relaxation strategies to keep your mind from focusing on the pain.
diet
Some diets are highly inflammatory, especially those high in trans fats, refined sugars, and processed foods. Consult your doctor to find out if your diet could be contributing to chronic back pain and how you can change it. Maintaining a healthy weight can also help reduce back pain by reducing pressure on your spine.
Lifestyle modifications
When you have chronic pain, it’s important to accept your limitations and adapt to them. Listen to your body and learn to regulate yourself. Take breaks when mowing the lawn, or take several trips when carrying groceries. Note the activities that aggravate the pain and avoid them if possible. It doesn’t help. It can help not only improve your back, but it can also prevent the underlying condition from progressing. Another important lifestyle change to try is to quit smoking. It is scientifically known that nicotine increases pain and delays recovery.
Injection-based therapies
Nerve blocks, epidural steroid injections, nerve ablations, and other types of injection-based procedures are available for chronic back pain. These are used when the source of the pain is known and can sometimes help rule out certain causes. If treatment doesn’t work, the injections may stop or relieve the pain for a while. certain period of time, but are not intended to be long-term solutions and should not be used in isolation.
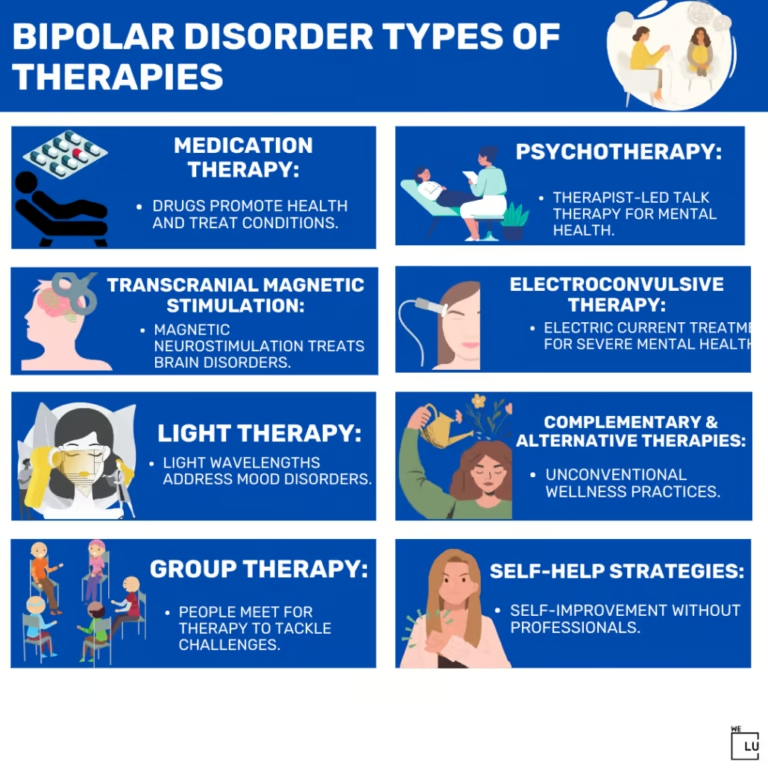
Alternative therapies
Acupuncture, massage, biofeedback therapy, laser therapy, electrical nerve stimulation and other non-surgical spine treatments can make a difference for chronic back pain. Talk to your spine specialist about alternative therapies that may work for you.
Pharmacological treatments
Analgesics, anti-inflammatory drugs, muscle relaxants, and other medications can be used to help control chronic back pain. However, most of them come with unwanted side effects and are not intended for prolonged use.