Antibiotics are among the most commonly prescribed medications, with more than 236 million prescriptions written in the United States in 2022, according to the Centers for Disease Control and Prevention (CDC).
Antibiotics are among the most commonly prescribed medications, with more than 236 million prescriptions written in the United States in 2022, according to the Centers for Disease Control and Prevention (CDC) . This equates to roughly seven prescriptions for every 10 people in outpatient care. While these medications are essential for fighting bacterial infections, they can also throw the digestive system off balance in ways patients don’t always anticipate. If you’ve started taking such a prescription and suddenly feel like your stomach is sluggish, there may be an explanation.
Below, Linda Yancey, MD, a board-certified infectious diseases physician at Memorial Hermann Hospital in Houston, reveals whether your antibiotic could be linked to constipation and what happens to your digestive system when you take antibiotics.
Do antibiotics cause constipation?
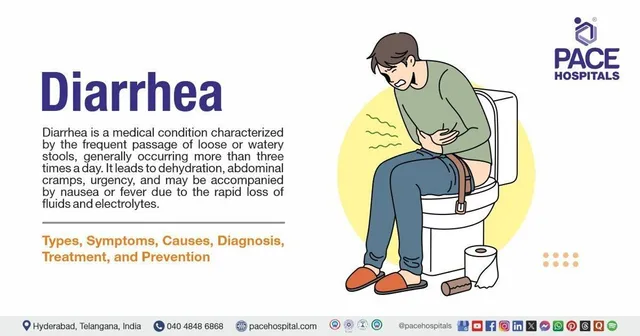
“Antibiotics don’t cause constipation,” says Dr. Yancey. “Rather, their main side effect is diarrhea.”
This is because the gut is home to trillions of bacteria that aid digestion and maintain bowel regularity. “Up to 40% of stool volume is bacteria. When people take antibiotics, they wipe out these beneficial bacteria that help us digest food,” she explains. This disruption to the gut microbiome can throw digestion off balance, often resulting in softer stools instead of constipation.
In some cases, antibiotic use can lead to a more serious complication caused by a bacteria called Clostridioides difficile (often referred to as “ C. diff” by healthcare professionals). Dr. Yancey says that C. diff “can cause severe diarrhea that often requires hospitalization.”
C. diff infection can cause symptoms such as watery diarrhea, fever, loss of appetite, nausea, and abdominal pain. People at greatest risk include older adults, people with weakened immune systems, and those who have recently been hospitalized or undergone prolonged antibiotic treatment.
If you experience persistent diarrhea after taking antibiotics, it is important to seek medical attention immediately.
Other reasons you may experience constipation when taking antibiotics
Although antibiotics alone don’t cause constipation, you may experience it while taking these medications. In most cases, constipation is due to other factors related to the illness or changes in routine.
Possible causes of constipation while taking antibiotics include:
- Dietary Changes: When people aren’t feeling well, they often eat fewer fiber-rich foods, such as fruits, vegetables, and whole grains, which can slow digestion. It’s natural to want to take care of your body when you’re not at your best, but when you start to feel better, Dr. Yancey says it’s important to know: “Fresh fruits and vegetables are very important for good gut health. The gut microbiome isn’t fully understood, but we’re starting to realize that the foods we eat can have a profound effect on these bacteria.”
- Dehydration: Not drinking enough water can make stools harder and harder to pass.
- Reduced physical activity: Being sick can mean spending more time resting and less time moving, which is good for recovery, but can also slow down digestion.
- Other medications: Pain relievers, antihistamines, and certain antacids can contribute to constipation.
How to relieve constipation
If you’re feeling stuck, try these simple remedies to help get things moving:
Drink more water
Hydration is key to maintaining healthy digestion. Warm liquids, such as herbal teas or warm lemon water, can also help stimulate bowel movements.
Increase your fiber intake
A diet rich in fiber can help regulate digestion and promote bowel regularity. Whole grains (such as oats, brown rice, and whole-wheat bread), fresh fruits (such as pears, apples, and berries), and vegetables (including leafy greens, carrots, and broccoli) provide the fiber needed to maintain good health. Legumes, such as beans and lentils, are also excellent sources of fiber.
Get moving
Regular physical activity can stimulate the digestive tract and help relieve constipation. Even light exercise, such as a 15- to 30-minute walk, can promote bowel movements. Yoga postures for the bowel, such as those involving twisting movements, can also be beneficial for promoting digestion.
Try a natural remedy
Prunes and their juice are recognized as natural laxatives due to their high fiber and sorbitol content. Other natural options include flax seeds, chia seeds, and probiotics, which promote a healthy gut microbiome.
Consider a mild laxative
If constipation persists despite dietary and lifestyle changes, an over-the-counter osmotic laxative like Miralax can help draw water into the intestines, making stool easier to pass. Stool softeners and fiber supplements, such as psyllium husk (Metamucil), can also be effective. However, always consult your doctor before using any laxative, especially if you are taking antibiotics or other medications.
You might be interested in: Should you take digestive supplements for your gut health?
How else can antibiotics affect your digestion?
Although constipation is not a side effect, antibiotics can cause other digestive problems, including:
- Diarrhea: This is the most common digestive side effect of antibiotics. “Almost everyone who takes antibiotics will have loose stools,” says Dr. Yancey.
- Nausea: Some antibiotics irritate the gastric mucosa, causing nausea, especially if taken on an empty stomach. Eating a light meal before taking antibiotics can help minimize this effect.
- Gas and bloating: Because antibiotics disrupt the gut microbiome, they can cause temporary imbalances that result in excessive gas production and bloating.
- Abdominal cramps: Changes in gut bacteria and stool consistency can sometimes cause mild cramps.
When to see a doctor
If you suffer from persistent constipation that doesn’t improve with home remedies, it’s important to consult your doctor. Seek medical attention if you experience any of the following symptoms, among others:
- Constipation that lasts more than a few days
- Severe abdominal pain or bloating
- Blood in the stool
- Inability to pass gas or stool